An Unusual Localization for A Proximal Median Nerve Lesion: Case Report and Review of the Literature
Author(s): ALI H SREIJ, RAJA SAWAYA
*Corresponding author: Sreij AH, Department of Neurology, Clinical Neurophysiology laboratory, American University of Beirut Medical Center, Beirut, Lebanon, E-mail: asreij10@gmail.com
Citation: Sreij AH, Sawaya R (2024) An unusual localization for a proximal median nerve lesion: case report and review of the literature. Clin Img and Med Case Rep Vol.1 No. 1
Copyright: ©2024 Sreij AH. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
We report a patient who presented with the classical picture of carpal tunnel syndrome, but had a normal nerve conduction study across the wrist. She later developed weakness of the flexor pollicis brevis muscle. Extensive nerve conduction studies confirmed a lesion of the motor fibers of the median nerve at the distal part of the medial cord, before the anastomosis with the lateral cord and distal to the branch that becomes the ulnar nerve. The patient did not report any trauma or fall or compression or traction or surgery on the arm. All investigative study failed to reveal an etiology. Repeated nerve conduction study confirmed the lesion. After a course of steroids, the patient was cured and the nerve conduction studies normalized. We describe an idiopathic, proximal median nerve lesion with a rare localization
Introduction
The most common mononeuropathies in adults occurs in the median nerve. Entrapment of the median nerve is most frequent in the carpal tunnel and occurs much less at the elbow or in the brachial plexus (1). Etiologies for median mononeuropathies are frequent and usually easy to diagnose. Causes can range from focal entrapment, compression, trauma, traction, tumors, hematomas, aneurysms, infections, toxic, iatrogenic and other rare causes (1,2). Idiopathic mononeuropathies of the median nerve are very rare.
Frequently patients with a mononeuropathy of the median nerve present first with numbness in the first three digits of the involved hand followed by weakness in hand grip secondary to involvement of the abductor pollicis brevis and opponens muscles. The diagnosis is confirmed by nerve conduction studies of the median and ulnar nerve at the wrist. In few occasions the diagnosis is missed specifically for the reason that the nerve conduction study is limited to the wrist and not extended proximally to enable the study of the median nerve as a whole (2).
Case Report
We describe a middle-aged woman presenting with the classical clinical picture of a right-sided carpal tunnel syndrome. Nerve conduction studies were reported as normal, but it is important to point out that the study was limited to the level of the wrist. The patient was labelled as functional and started on selective serotonin reuptake inhibitors.
Ten days later, the patient developed further numbness and weakness in the median myotome of the right hand, and sought a second opinion. A neurologic examination confirmed weakness of the right abductor policis brevis as well as the flexor policis longus.
A more extensive nerve conduction study was performed including proximal segments up to the level of Erb’s point. Fractionated motor neurography of the right median nerve revealed a 50% drop in the compound muscle action potential (CMAP) upon stimulating at the axilla, and supraclavicular fossa in comparison to stimulation at the elbow and the wrist. There was also a 50% drop in the conduction velocity between the axilla and the elbow in comparison the velocity in the forearm between the elbow and the wrist (Figure1A) (Table 1).
Electromyography revealed fibrillations, and positive sharp waves in the right pronator teres, flexor digitorum of the median nerve, flexor policis longus, and abductor policis brevis. Few neurogenic motor units were seen in the right flexor policis longus, and abductor policis brevis muscles. Normal EMG with absence of spontaneous activity in the triceps, biceps, radial, and ulnar innervated forearm, and hand muscles.
Sreij AH, et al.
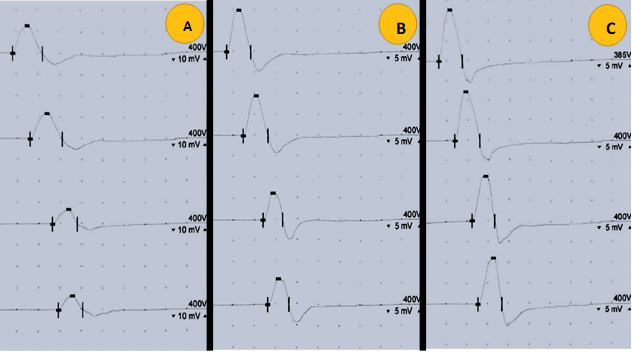 Figure 1: The fractionated compound motor action potentials of the right median nerve at the wrist, elbow, axilla, and Erbs point. A: February 2, 2024, B: February 26, 2024, C: March 26, 2024.
Figure 1: The fractionated compound motor action potentials of the right median nerve at the wrist, elbow, axilla, and Erbs point. A: February 2, 2024, B: February 26, 2024, C: March 26, 2024.
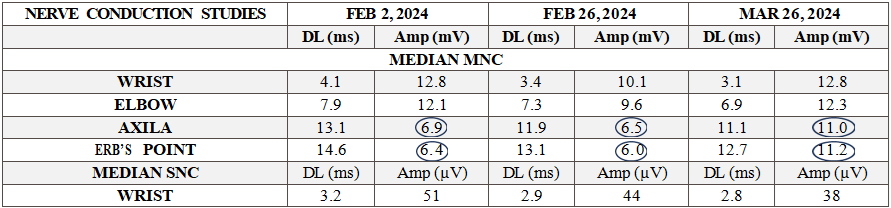
Table 1: The nerve conduction studies of the motor and sensory fibers of the median nerve on the different dates.
Fractionation of the ulnar and radial motor nerve did not reveal any conduction block or slowing. Nerve conduction studies of the left arm and the lower extremities were normal. It is important to note that the sensory responses in the median, ulnar, and radial nerves were normal and symmetrical bilaterally. The patient was diagnosed with an isolated focal motor mononeuropathy of the right median nerve above the elbow at the terminal region of the brachial plexus (Figure 2).
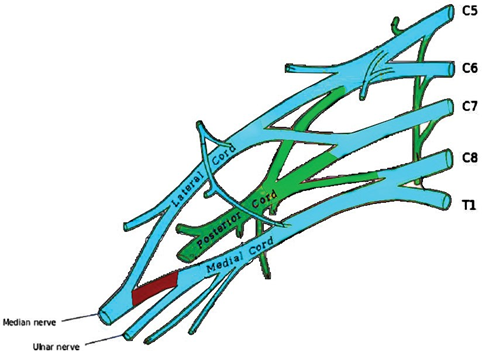
Figure 2: The localization of the lesion in the right brachial plexus.
The patient was started on intravenous high dose methylprednisolone 1g per day for three consecutive days followed by oral steroids with tapering dose over three weeks.
Three weeks later, the patient described partial improvement in the numbness and weakness in the right hand. A repeat nerve conduction studies showed no change in the conduction block, decreased CMAP amplitudes, and decreased conduction velocity in comparison to the pre- steroids study (Figure 1B) (Table 1). The patient was kept on steroids and sent to physical therapy and exercises.
One month later, the patient presented to the clinic. Her numbness subsided and she had normal motor power of all the muscles of her hand and forearm. A control nerve conduction study was performed which showed normalization of the fractionated median motor neurography with no drop in CMAP amplitude or the conduction velocity (Figure 1C) (Table 1).
The diagnosis of isolated, reversible, idiopathic, focal nerve lesion was entertained. No etiology could be elicited. Recovery was complete with time and steroids. No generalized neuropathy could be confirmed. The lesion is suspected to be exactly proximal to the anastomosis of the lateral cord (median sensory fibers) and medial cord (median motor fibers) at the level of the arm. The lesion is distal to the branching of the ulnar nerve from the medial cord (Figure. 2).
Discussion
The most common mononeuropathy in adults is the median nerve. The most frequent entrapment region for the median nerve is the carpal tunnel. Only 0.2% of the patients with median nerve pathology have the lesion proximal to the carpal tunnel (1).
Median nerve compression can be caused by many pathologies. Entrapment in the carpal tunnel is seen in hypothyroidism, obesity, pregnancy, and manual labor (2).
The rare cases of median nerve mononeuropathy outside the carpal tunnel is reported as anecdotal case reports because of its infrequent occurrence. Idiopathic mononeuropathy of the median nerve in the arm has been reported to be associated with the abnormal presence of the superficial brachial artery. The incidence of this anatomical anomaly in the different populations ranges from 0.12% to 19.7% (3).
Infections of the forearm and hand usually affect the median and ulnar nerves simultaneously except in rare conditions such as leprosy where the neuropathy is isolated to one of the nerves (4). In these circumstances, the infection involves the motor and sensory fibers of the nerve involved.
Toxins and metabolic disorders cause neuropathies, but these are usually sensorimotor and involve multiple nerves with a distal predilection. These are seen in diabetic patients, patients with chronic renal failure on dialysis, patients on chemotherapy, and neurotoxins such as drugs, nitrofurantoin or amiodarone, bacteria such as diphtheria and lead poisoning.
Isolated median mononeuropathy has been reported by the jellyfish toxin causing a demyelinating lesion which recovers spontaneously with time. The lesion reported is in the forearm and not above the elbow as in our case. The reported case recovered spontaneously suggesting a reversible conduction failure rather than a conduction block as in our patient requiring immunotherapy (5).
Proximal median nerve injuries above the elbow, around the brachial plexus, or the supraclavicular fossa has been frequently reported in patients following blunt or penetrating trauma, motor vehicle accidents, nerve transection, tumors, hematomas, traction injuries, and not infrequently iatrogenic injuries during surgery in the region of the brachial plexus (1). Positioning and traction during surgery, shoulder adduction, and stretching during sternotomy have been associated with isolated iatrogenic nerve injuries in the arm particularly the median nerve (1,6,7).
When authors report proximal median nerve injuries, they usually refer to injuries in and around the region of the elbow. Frequent publications report on isolated proximal median neuropathy seen after prolonged compression on the forearm in patients intoxicated with alcohol. The lesions are usually located below the inferior border of the pectoralis major muscle, and involves the motor and sensory fibers. The pathology is usually a neuropraxia with spontaneous resolution overtime (6,7).
What is specific in the case we are presenting is that our patient does not give any history of an infection, trauma, traction, surgery, or compression of the arm or hand. The symptoms presented spontaneously. The nerve conduction studies confirm, in two separate occasions, an isolated lesion of the median nerve involving only the motor fibers. The pathology was both a demyelinating block and early motor axonal degeneration. The localization and pathology were confirmed by the nerve conduction studies twice to be at the distal level of the brachial plexus, in the medial cord, distal to the bifurcation of the ulnar nerve (Figure 2). The MRI of the brachial plexus could not delineate any morphologic abnormality. Systemic investigations and CSF studies could not confirm any systemic illness, polyneuropathy or mononeuritis multiplex.
Whether the patient improved spontaneously or after steroid treatment is difficult to assess, but the improvement in a matter of weeks suggest a benign etiology. The interesting aspect of this case is the unusual localization, lack of etiology, isolated motor involvement, and fast recovery.
The case also confirms the importance of performing extensive nerve conduction studies in controversial cases rather than quickly attributing the symptoms to functional derangements.
Conflict of Interest
Authors declare no conflict of interest.
Funding
No Funding.
References
- Chen YY, Huang CC, Wang JC, Hsu PC. (2022) Isolated Proximal Median Neuropathy after Aortic Dissection Repair: Case Report. Medicina (Kaunas) 58:622.
- Kanaan N, Sawaya RA (2001) Carpal tunnel syndrome: modern diagnostic and management techniques. Br J Gen Pract 51: 311-314.
- Nkomozepi P, Xhakaza N, Swanepoel E. (2017) Superficial brachial artery: a possible cause for idiopathic median nerve entrapment neuropathy. Folia Morphol (Warsz) 76: 527-531.
- Vital RT, Illarramendi X, Antunes SL, Nascimento M, Da Costa Nery JA, Nascimento O,et al. (2013) Isolated median neuropathy as the first symptom of leprosy. Muscle Nerve 48: 179-184.
- Al-Ajmi AM, Jayappa S, Rousseff RT. (2013) Isolated severe median mononeuropathy caused by a jellyfish sting. J Clin Neuromuscul Dis 14: 188-193.
- Roth G, Ludy JP, Egloff-Baer S. (1982) Isolated proximal median neuropathy. Muscle Nerve 5: 247-249.
- Isaacs J, Ugwu-Oju O. (2016) High Median Nerve Injuries. Hand Clin 32: 339-348.

