Metatypical Basal Cell Carcinoma: Report of A Case with Granular Cell Change
Author(s): RAMTIN EDJTEMAEI
*Corresponding author: Dr. Ramtin Ejtemaei, MD, AP,CP, pathology laboratory, Razi hospital, Guilan University of Medical Sciences, Sardar Jangal boulevard, Rasht Iran, Tel: +989112366498, Email: Ramtin.ir.edjtemaee@gmail.com
Citation: Edjtemaei R (2024) Metatypical Basal Cell Carcinoma: Report of A Case with Granular Cell Change. Clin Img and Med Case Rep Vol.1 No.1:1
Copyright: ©Edjtemaei R. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Granular cell Basal cell carcinoma (BCC) is an extremely rare variant of BCC which was first reported in 1979. Granular cell BCC is characterized by large cells with abundant eosinophilic and granular cytoplasm and eccentrically located nucleus. Metatypical BCC is another rare variant of BCC, composed of nests and cords of cells, with moderate squamous maturation. A 43 y/o woman presented with an ulcerated lesion of upper lip. The lesion underwent surgical excisional biopsy. Microscopic examination revealed skin tissue heavily infiltrated by basaloid tumor cells, arranged in nests with peripheral palisading and cleft formation, consistent with basal cell carcinoma, as well as focal squamous differentiation and granular cell change. Tumor cells expressed Ber-EP4 and CK5,6, but showed negative reaction for S100 on immunohistochemical study. Tumor cells with granular cell change also expressed CD68. This subtype of BCC is rare and granular cell change can also occur in other neoplasms. Definite diagnosis would be difficult if no relationship is seen between tumor cells and surface epidermis or prepared sections do not contain conventional BCC, so pathologists ought to be familiar with this subtype of BCC for appropriate diagnosis.
Keywords
Granular Basal cell carcinoma, metatypical basal cell carcinoma, Ber-EP4, CK5,6, CD68, S100, Immunohistochemistry
Introduction
Basal cell carcinoma is the most common primary skin neoplasm which is responsible for nearly 70% of skin malignancies(1). Different morphologic subtypes of this neoplasm have been reported in the literature. Granular Basal cell carcinoma (BCC) is a very rare variant of BCC which was first reported in 1979(2). A total number of 17 cases of this subtype have been reported in the literature to date. Granular cell BCC is characterized by large cells with abundant eosinophilic and granular cytoplasm and eccen- trically located nucleus.

Figure 1: Ulcerated and crusted skin lesion of upper lip with irregular borders.
In this study, we are about to present a case of BCC with both metatypical and granular cell change.
Case history
A 43 y/o woman without previous past medical history, presented with a nevus-like lesion of the upper lip from 12 years ago. Surgical excision for cosmetic reasons was per- formed twice that ended in relapse after four years (unfor- tunately no pathology report was available). An ulcerated lesion, rapidly growing in size, developed in surgical site (Figure 1). The patient was referred to the dermatologic cancer clinic of Razi Dermatology Hospital, Tehran, Iran and a surgical incisional biopsy with clinical impression of Squamous cell carcinoma was performed and the specimen was sent to the pathology department for histopathologic evaluation. The primary pathology report at this center was in favor of Basal cell carcinoma, solid type. The patient underwent surgical excisional biopsy.
Investigations:
The submitted sample consisted of a piece of creamy tan skin tissue, measuring 3x2.5x1.5cm. At the center of the specimen, an ulcerated lesion was seen measuring 2.7x2.3cm, which was slightly depressed and was covered by a thick brownish crust. Representative sections were fixed at 10% formalin, and serially dehydrated in graduated alcohols and embedded in paraffin. Sections were stained by Hematoxylin & Eosin method. Representative sections for immunohistochemical evaluation were stained by Avi- din-Biotin-Peroxidase complex method and antibodies against the following antigens were directed: Ber-EP4, CK5,6, S100 and CD68. Two expert dermatopathologists evaluated the prepared slides. Microscopic examination revealed basaloid tumor cells that were arranged in nests, with deep dermal infiltration. Tumor composed of cells with large round nuclei and occasional prominent nucleoli and scant cytoplasm with peripheral palisading and cleft formation between tumor cells and adjacent stroma, in- dicating basal cell carcinoma. Focal growth of neoplastic cells with moderate amounts of eosinophilic cytoplasm, presenting mixed features of Basal cell carcinoma and Squamous cell carcinoma, without significant keratiniza- tion (1, 3) was also noted. Some of the tumor nests revealed granular cell change at the center that were surrounded by basaloid tumor cells at the periphery. Numerous eosino- philic round cytoplasmic inclusions were present in gran- ular cells (Figure 2). All inked surgical margins were free from tumor. Immunohistochemical examination revealed diffuse positive reaction for Ber-EP4 (strong membranous and cytoplasmic) and CK5,6 (strong membranous and cytoplasmic), in conventional BCC as well as areas with metatypical change and granular cell change. Tumor cells with granular cell change also focally expressed CD68. All neoplastic cells (including cells with granular change) showed negative results for S100 protein (Figure 3).
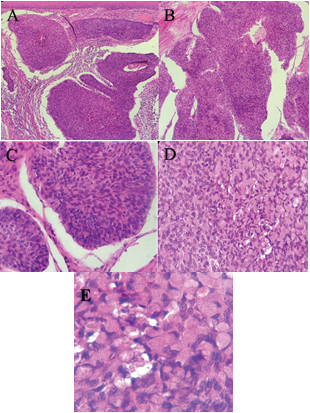
Figure 2: A) Low power section showing skin tissue infiltrated by basaloid tumor, with typical peripheral palisading and tumor- stromal clefting, metatypical change at left and top and granular cell change at the bottom.
B) High power section of Basal cell carcinoma showing squamous differentiation (metatypical change).
C and D) Basal cell carcinoma with Granular cell change in center surrounded by basaloid tumor cells in periphery.
E) High power section of granular cell BCC with abundant eosinophilic and granular cytoplasm and eccentrically located nucleus
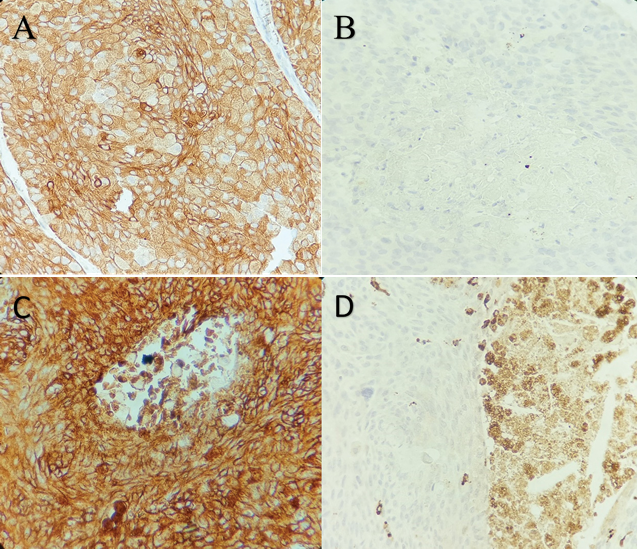
Figure 2: A) Immunohistochemical study for CK5,6 , showing positive result with diffuse cytoplasmic and membranous staining.
B) Negative staining for S100 protein in both conventional BCC and areas with granular cell change in center.
C) Diffuse positive reaction for Ber-EP4 in both conventional BCC and areas with granular cell change in cente.
D) Positive reaction for CD68 in areas with granular cell change, and rather negative results in peripheral basaloid tumor cells.
Discussion
Basal cell carcinoma is the most common prima- ry skin neoplasm. Many histopathologic subtypes of this neoplasm have been described in the literature, including nodular, superficial multifocal, cystic, infiltrating, sclerotic, pigmented, keratotic and metatypical types(1). Metatypical and infiltrating types are known to have more aggressive clinical behavior and are accompanied by higher incidence of relapse and metastasis (1).
Ber-EP4 is a cytoplasmic and membranous marker of nearly all epithelial cells except normal keratinocytes, he- patocytes and parietal cells of the stomach. This marker is also positive in BCC(1), which can help distinguish this tumor from other neoplasms in differential diagnosis, in- cluding squamous cell carcinoma, which is always negative for this marker(1). Basal cell carcinomas also reveal positive reactions for Cytokeratins, including LMWCK and HM- WCK, CKAE1/E3 and CK (4). All BCCs with granular cell change typically express the above markers(5), as revealed in our case, tumor cells were positive for CK5,6. Specifically granular cells may be positive for CD68, as shown in our case Edjtemaei R.
Granular cell change happens extremely rarely in BCC. Although it is believed, tumors with granular cell change behave the same as conventional BCC (6) and patients’ out- comes are not different from ordinary BCC, it is import- ant to keep this rare variant in mind since granular cell change occurs in other neoplasms in differential diagno- ses. Granular cell change is reported in both benign con- ditions (including Angiofibroma, Ameloblastoma, Gran- ular cell tumor and Leiomyoma) and also in malignant neoplasms (including Angiosarcoma, Leiomyosarcoma, Dermatofibrosarcoma protuberans, Melanoma and ma- lignant peripheral nerve sheath tumor)(7). Rather than this, definite diagnosis of granular cell BCC may be challeng- ing if the tumor lacks epidermal attachment or areas with conventional BCC (6). Immunohistochemical staining for S100 protein can help distinguish BCCs with granular cell change from some of the differential diagnoses mentioned above, which is typically negative in BCC with granular cell change, but positive in Granular cell tumor(8) and Mel- anoma and may be focally positive in Malignant peripheral nerve sheath tumor (MPNST).
In the presented case, we described an extremely rare case of basal cell carcinoma of the upper lip in a mid- dle-aged woman with both metatypical and granular cell changes. The diagnosis was also confirmed by immuno- histochemistry (IHC). Although the present case did not show relapse as far as followed, Metatypical BCC directly correlates with higher incidence of relapse, local extension and metastasis, so close follow-up of the patients after com- plete resection of the tumor is recommended. Granular cell BCCs are efficiently treated with complete resection and the patient outcome is the same as conventional BCC. Pa- thologists may need to exclude other neoplasms with gran- ular cell change when encountering this histomorphology. IHC study may be helpful for the mentioned purpose.
Author contributions
References
Dr Ramtin Ejtemaei was responsible for data preparation, original draft writing, supervision and editing. Dr Kambiz Kamyab and Dr Sahar Montazeri prepared consultation, supervision and revision.
Acknowledgement
The authors of this case report would like to thank Dr Fereshte Ameli, pathologist, MD, AP, CP, for her generous financial support of immunohistochemical preparations.
Ethics approval and consent to participate:
All procedures were performed in accordance with the 1964 Helsinki Declaration and its latest amendments. Informed written consent was obtained from the patient’s offspring (the patient’s son, since the patient was not alive at the time of performing this case report). Patient’s per-sonal information including identity and face pictures was never published anywhere.
Consent for publication
Written informed consent was obtained from the pa- tient in accordance with the journal’s patient consent policy.
Funding
The authors received financial support for immunohis- tochemical study from Dr Fereshte Ameli, pathologist and assistant professor of Tehran University of Medical Sciences. Other technical procedures, authorship, and publication of this article had no funding.
Conflicts of interest:
All authors declared that there are no conflicts of in- terest
Data availability statement
All data that support the findings of this study are avail- able at corresponding author and would be delivered upon reasonable request.
- Weedon D (2009) Weedon’s Skin Pathology E-Book: Expert Consult-Online and Print: Elsevier Health Sciences.
- Barr RJ, Graham JH (1979) Granular cell basal cell carcinoma: a distinct histopathologic entity. Archives of dermatology 115: 1064-1067.
- Cardoso J, Wollina U, Tchernev G (2017) Ulcerated Metatypical Basal Cell Carcinoma of the Forehead. Open access Macedonian journal of medical sciences 5: 807-809.
- Pahnke T-M, Schmidt U, Bug R (1997) Granular Cell Basal Cell Carcinoma and Granular Cell Tumor-Light Microscopic and Immunohistochemical Comparison. The American Journal of Dermatopathology 19: 428.
- Boscaino A, Tornillo L, Orabona P, Staibano S, Gentile R, De Rosa G (1997) Granular cell basal cell carcinoma of the skin. Report of a case with immunocytochemical positivity for lysozyme. Tumori Journal 83: 712-714.
- Claassen SL, Royer MC, Rush WL (2014) Granular cell basal cell carcinoma: report of a case and review of the literature. The American Journal of Dermatopathology 36: e121-e124.
- Dundr P, Štork J, Povýšil C, Vosmík F (2004) Granular cell basal cell carcinoma. Australasian journal of dermatology 45: 70-72.
- Ma X, Wang G, Kuwadekar A, Zhao M, Hu W, Wu Y, et al. (2018) Granular cell basal cell carcinoma: a case report. Journal of cutaneous pathology 45: 223-225.

