Takotsubo Syndrome Associated with Acute Ischemic Stroke Following Therapy with Intravenous Alteplase
Author(s): ANDREAS LIAMPAS, DIMITRIS ORESTIS PAVLOU, MICHAELA KYRIAKOU, GEORGIOS M HADJIGEORGIOU, PANAGIOTIS BARGIOTAS
1Department of Neurology, Nicosia New General Hospital, Nicosia, Cyprus
2University of Thessaly, Larisa, Greece
3Department of Cardiology, Nicosia New General Hospital, Nicosia, Cyprus
4Medical School, University of Cyprus
*Corresponding author: Andreas Liampas, Department of Neurology, Nicosia New General Hospital, Nicosia, Cyprus, Tel: +357 2260 3911; E-mail: liampasand@gmail.com
Citation: Liampas A (2024) Takotsubo Syndrome Associated with Acute Ischemic Stroke Following Therapy with Intravenous Alteplase. Clin Img and Med Case Rep Vol.1 No.2
Copyright: ©2024 Liampas A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Dear Editor
Takotsubo syndrome (TTS), also known as apical ballooning syndrome, stress-induced cardiomyopathy or broken heart syndrome, is an acute and reversible cardiomyopathy characterized by acute transient left ventricular (LV) dysfunction describing as left ventricular end-systolic apical ballooning phenomenon [1]. TTS is estimated to account for approximately 1–3% of patients presenting with suspected myocardial infarction [2]. TTS is usually induced by physical or psychological stress and typically presented with acute chest pain, dyspnea or syncope, electrocardiogram (ECG) changes and elevation of plasma levels of cardiac proteins mimicking acute myocardial infarction (AMI) [2]. The exact pathophysiological mechanism remains unknown, though the process seems to be multifactorial. Many reports of TTS event have been described following stroke. Here, we report a case of TTS following treatment with intravenous alteplase for acute ischemic stroke (AIS).
A right-handed female at her 60s was admitted to our emergency department after experiencing acute onset dizziness following dysarthria with right-sided weakness involving the upper and lower limb. Past medical history included hypertension. The contrast computer tomography angiography (CTA) of the brain and the neck was normal. The patient had a National Institutes of Health Stroke Scale (NIHSS) score of 8 points and treatment with intravenous administration of alteplase was initiated. During the thrombolytic therapy, the patient complained of atypical chest pain. The cardiovascular and respiratory examination was unremarkable. The electrocardiogram (ECG) taken during ongoing chest pain, demonstrated dynamic changes with ST-segment elevation in V1-3, though cardiac enzymes and troponin levels were normal.
Chest x-ray demonstrated clear lung fields. After the thrombolytic treatment, the patient had no neurological deficit. A few hours later, the patient complained of chest pain and an ECG showed giant T-wave inversion in V3-6 and blood chemistry showed elevated troponin levels of 5.17 ng/ml. TTE showed apical ballooning and akinesia of apical segments of left ventricle with hypercontractility of basal segments and a decreased systolic function with an ejection fraction (EF) 40-45%. No thrombus was seen in the apex of left ventricle (LV). The next day she underwent a coronary angiogram, which revealed unobstructed coronaries and the left ventriculography showed impaired left ventricular function with severe hypokinesis, akinesis of the apical wall, and the diagnosis of TTS was confirmed (Figure 1). Magnetic resonance imaging of the brain revealed a small infarct on the left parietal periventricular area (Figure 2). A few days later, the patient was discharged without any neurological deficit. The patient remained asymptomatic over 1 year of follow-up.
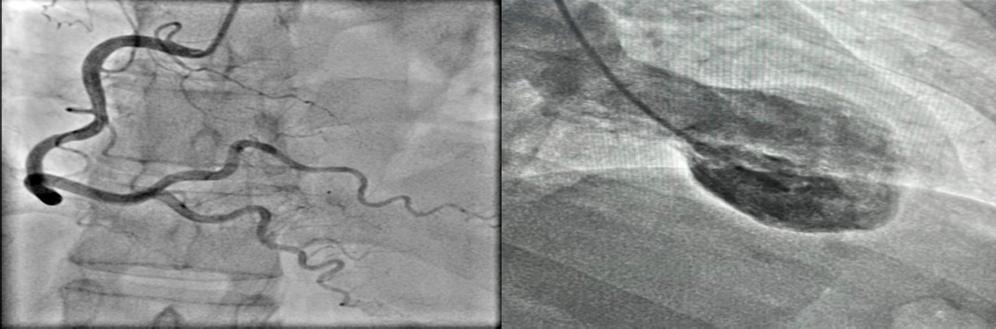
Figure 1: Coronary angiogram; unobstructed coronary arteries on the left and systolic ballooning of the apex and hypercontraction of the basal segment with akinesis of the apical wall on the right.
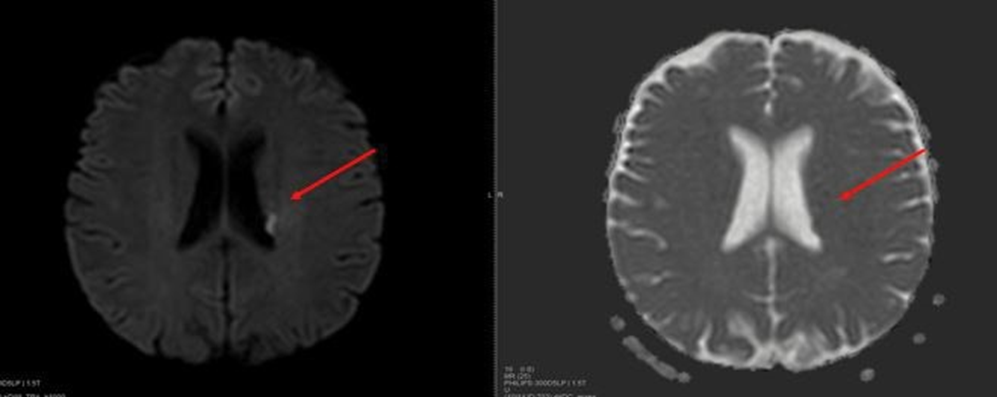
Figure 2: Ischemic lesion in the left parietal periventricular area 24 hours after the thrombolytic therapy with intravenous alteplase.
In this report, we present for the first time a case of TTS in a patient with AIS after thrombolytic treatment with intravenous alteplase. Neurological diseases including AIS are some of the most common physical triggers for TTS. Following a stroke, myocardial ballooning usually develops within the next 10 hours [3]. The association between stroke and TTS is bidirectional and, in some cases, it may be difficult to establish which of these events occurred first. Stroke could serve as a type of physical stress that leads to TTS and TTS could cause embolic strokes. Despite recent progress, TTS pathogenesis has not been clearly identified yet. The most widely accepted theory regarding the pathogenesis of TTS is that of catecholamine surge. According to this theory, a physically or emotionally stressful event leads to the release of catecholamines and to the development of TTS. Catecholamine levels may increase via stimulation of the hypothalamic- pituitary-adrenal axis or via increased local cardiac release from efferent sympathetic nerves. Therefore, catecholamine surge can be the result of an increased systemic catecholamine concentration or an amplified local catecholamine release [4]. Closely related with the catecholamine surge hypothesis for TTS pathogenesis, is the theory of brain-heart axis malfunction. The nervous system is crucial in the development of TTS. The central autonomic network plays a crucial role in the regulation of cardiovascular functions via various mechanisms. Brain MRI studies of TTS patients revealed both structural and functional abnormalities, mainly in the limbic system, with reduced cortical thickness, hypoconnectivity and abnormal responses of areas responsible for emotional processing and the autonomic nervous system [5]. Regions such as the amygdala, the hippocampus, the cingulate gyrus and the insular cortex are among those affected. Interestingly, the absence of an emotional trigger is common in these patients and the left insular ischemic infarcts are the most strongly associated with TTS. The insular region is involved in the regulation of cardiac function and damage in this area can lead to autonomic dysregulation, a common result of brain- heart axis damage [5]. The insular region is involved in the regulation of cardiac function and damage in this area can lead to autonomic dysregulation, a common result of brain-heart axis damage. In conclusion, we suggest that the ischemic stroke can serve both as a sympathetic nervous system stimulatory trigger and as a proinflammatory event, both of which are potential mechanisms of TTS.
Statements and Declarations
The authors declared no conflicts of interest with respect to the authorship and/or publication of this article.
Competing Interests and Funding
The authors received no financial support for the research and/or authorship of this article.
Compliance with Ethical Standards
Consent was obtained from the patient.
References
- Bairashevskaia AV, Belogubova SY, Kondratiuk MR, Rudnova DS, Sologova SS, Tereshkina OI, et al. (2022) Update of Takotsubo cardiomyopathy: Present experience and outlook for the future. Int J Cardiol Heart Vasc 39: 100990.
- Deshmukh A, Kumar G, Pant S, Rihal C, Murugiah K, Mehta JL (2012) Prevalence of Takotsubo cardiomyopathy in the United States. Am Heart J 164: 66–71.e1.
- Canavero I, Rifino N, Bussotti M, Carrozzini T, Potenza A, Gorla G, et al. (2022) The Octopus Trap of Takotsubo and Stroke: Genetics, Biomarkers and Clinical Management. J Pers Med 12: 1244.
- Kume T, Kawamoto T, Okura H, Toyota E, Neishi Y, Watanabe N, et al. (2008) Local release of catecholamines from the hearts of patients with tako-tsubo-like left ventricular dysfunction. Circ J 72: 106-8.
- Hiestand T, Hänggi J, Klein C, Topka MS, Jaguszewski M, Ghadri JR, et al. (2018) Takotsubo Syndrome Associated With Structural Brain Alterations of the Limbic System. J Am Coll Cardiol 71: 809-811.

